Most people have heard of the low FODMAP diet, but how well do we understand what it can help with and how it should be implemented?
The low FODMAP diet is a three-phase dietary approach designed by researchers at Monash University, to help those with medically diagnosed irritable bowel syndrome (IBS) better manage their symptoms. Evidence suggests approximately 70–75 percent of people with IBS can experience symptoms from FODMAPs and following a low FODMAP diet can improve symptoms, especially bloating, abdominal pain, and diarrhoea. Some preliminary evidence suggests that limiting FODMAPs may also improve gut-related symptoms in those suffering endometriosis or inflammatory bowel disease, however more research is needed in this space.
WHAT IS A FODMAP ANYWAY?
FODMAPs are certain types of carbohydrates that are poorly digested in the small intestines but are rapidly fermented by gut bacteria once they reach the large bowel. FODMAP is an acronym, which stands for:
- Fermentable – carbohydrates that are broken down by gut bacteria.
- Oligosaccharides – fructans and galactooligosaccharides, found in foods such as legumes, wheat, and onions.
- Disaccharides – lactose, found in dairy products.
- Monosaccharides – fructose, found in certain fruits and sweeteners such as high-fructose corn syrup.
- And – no explanation needed for this one!
- Polyols – sorbitol, mannitol, xylitol and maltitol, found in certain fruits, vegetables, and artificial sweeteners.
WHAT’S ALL THE FODMAP FUSS ABOUT?
FODMAPs generate gas and have an osmotic effect, meaning they draw water into the intestines to help with gut motility, which prevents constipation. While this is all generally part of a healthy functioning digestive system, these processes can result in digestive issues for some people with sensitive guts. However, this doesn’t mean high FODMAP foods are bad for our health. In fact, healthy gut bacteria thrive on many high FODMAP foods and the majority of people can include these foods in their diets without any ill consequences. It’s important you don’t avoid FODMAPs unnecessarily, as many FODMAP-containing foods are a valuable part of a healthy dietary pattern. A low FODMAP diet actually reduces the abundance of beneficial bifidobacteria in the gut, and if poorly designed, can also reduce intake of fibre and certain micronutrients like iron and calcium, all of which are very important for our long-term health.
IS THE LOW FODMAP DIET RIGHT FOR YOU?
We need to understand that FODMAPs themselves are not the cause of IBS, so eliminating them won’t cure the condition. Also, the low FODMAP diet was never designed to be a permanent change; rather it is a tool to help people identify which particular foods and FODMAPs trigger their symptoms, allowing them to adopt a more suitable eating pattern in the long term, whereby healthy FODMAP foods are gradually reintroduced, so that the gut can learn to love them. As gastroenterologist Dr Will Bulciewicz likes to say, we can think of this process in a similar way to strength training, where the gut is a muscle that is becoming stronger through careful, incremental increases in intake.
Depending on a person’s baseline diet and lifestyle, other changes such as exercise, altering fibre intake, or reducing treat foods could be a more suitable starting point than a low FODMAP diet. Some people may see improvements in their symptoms simply by including more whole plant foods, eating slowly, managing their stress, or moving more. Trials have also found interventions like yoga and hypnotherapy to be just as effective as a low FODMAP diet for symptom management. Additionally, it’s worth noting that about 25 percent of IBS sufferers will not see improvements on a low FODMAP diet, so other therapies may need to be considered. When it has been determined that a low FODMAP diet is appropriate, there are three phases to move through:
- A two- to six-week elimination phase, where high FODMAP foods are swapped for low FODMAP alternatives.
- An eight- to 12-week reintroduction phase, where each FODMAP group is methodically reintroduced to help identify the specific FODMAPs that are causing symptoms and to establish tolerance levels.
- Personalisation is less of a phase and more for long-term health and symptom management. Well-tolerated FODMAPs should be included in the diet to promote diversity, while poorly tolerated foods remain restricted, but only to the level that provides symptom relief – the aim is to ease restrictions as much as possible!
IS LOW FODMAP AND PLANT-BASED EVEN POSSIBLE?
At first glance the initial phases of the low FODMAP diet may seem near impossible for plant-based people. Many healthy plant foods will need to be excluded in phase one but with a bit of planning, it is possible to achieve nutritional adequacy while eating this way as a vegan or vegetarian.
A common pitfall is removing too much fibre, which can result in constipation. Similar to a standard plant-based diet, when planning main meals, it’s helpful to include good wholefood sources of carbohydrate and protein, along with a variety of vegetables. Obtaining an adequate intake of certain micronutrients, such as calcium, iron, and omega-3, when following a plant-based, low FODMAP diet can also be a little challenging, so seeking advice from a dietitian or nutritionist is recommended.
LOW FODMAP NUTRIENT KNOW-HOW
CALCIUM
- Low-oxalate leafy greens, such as kale and rocket
- Chia seeds
- Tahini Calcium-set firm tofu
- Calcium-fortified plant milks, such as almond, cashew, or macadamia. If using soy milk, you will need to choose one made from protein isolates, not the whole beans.
IRON
- Pumpkin seeds
- Quinoa
- Oatmeal
- Tempeh
- Firm tofu
OMEGA-3
- Flax seeds
- Chia seeds
- Hemp seeds
- Walnuts
EAT AS MANY PLANT FOODS AS YOU CAN
People who consume more than 30 different plant foods per week have far greater microbial diversity, which supports good gut health, so try to include as many different whole plant foods as you can, even in phase one of the low FODMAP diet. It’s a great idea to purchase the Monash University FODMAP Diet app to help guide you in your food choices, as some foods have upper tolerable limits.
For example, small amounts of particular legumes are considered low FODMAP, but it is important to pay attention to serving sizes. Canned legumes have a lower FODMAP content than those cooked at home from dried legumes. This is because the water-soluble FODMAPs leach out of the legumes into the brine, therefore when the legumes are rinsed well before eating, less FODMAPs are consumed. Some people may still experience reactions to even small servings of legumes, so if this is the case for you, start by incorporating a very small serving, such as half a tablespoon of canned lentils, into a strictly low FODMAP meal. Slowly build on this quantity over a few weeks, while keeping track of symptoms.
While there are many fruits that will need to be avoided initially, there are still plenty of options to choose from. For example, cumquats, dragon fruit, grapes, guava, kiwi fruit (green and gold varieties), mandarins, papaya, and strawberries, to name a few. Low FODMAP varieties should actively be included as they are a good source of both soluble and insoluble fibre, which is important for regular bowel motions. Try to limit yourself to one serve of fruit per meal and aim for two serves per day. Again, check the Monash University FODMAP Diet app, as many other fruits can be included, just in smaller portions.
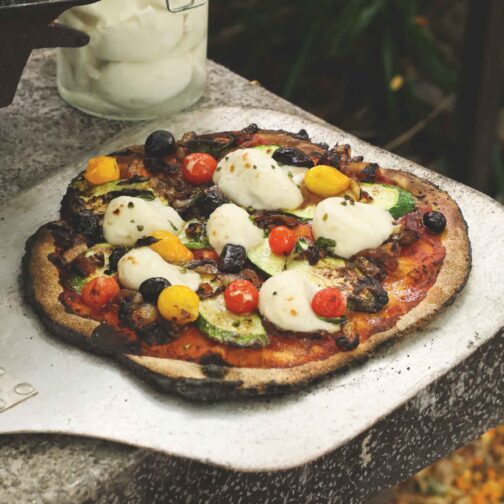
Rest assured, flavour can still be plentiful when eating low FODMAP – even though cooking without onion and garlic can seem like a tall order. You can still achieve delicious flavours with the use of low FODMAP herbs, spices, and condiments. Fresh herbs will be your best friend, so add basil, coriander, chives, lemon grass, mint, parsley, and rosemary to your meals, where appropriate. Dried herbs and spices such as cinnamon, cumin, paprika, and star anise will also be invaluable. And if you can’t get by without a hint of onion flavour, the green tops of spring onions are okay too. You can also add plenty of flavour with condiments such as mustards, peanut butter, tahini, soy sauce or tamari, capers, olives, tomato paste, nutritional yeast, and most vinegars.
A low FODMAP diet can offer symptom relief for the majority of people suffering from IBS, including vegans and vegetarians, but ultimately variety is key when it comes to a healthy gut microbiome. Remember, a low FODMAP diet can also reduce your intake of beneficial gut bacteria, particularly bifidobacterium species, therefore it’s vital to understand that this dietary regimen is not intended to be a permanent change. The goal should always be to liberate yourself to eat as many plant foods as possible, after doing the necessary detective work to find out your tolerable limits for specific trigger foods.
NOTE: A low FODMAP diet should be trialled under the guidance of a dietitian to avoid nutrient deficiencies, and after obtaining medical advice to establish a correct diagnosis.